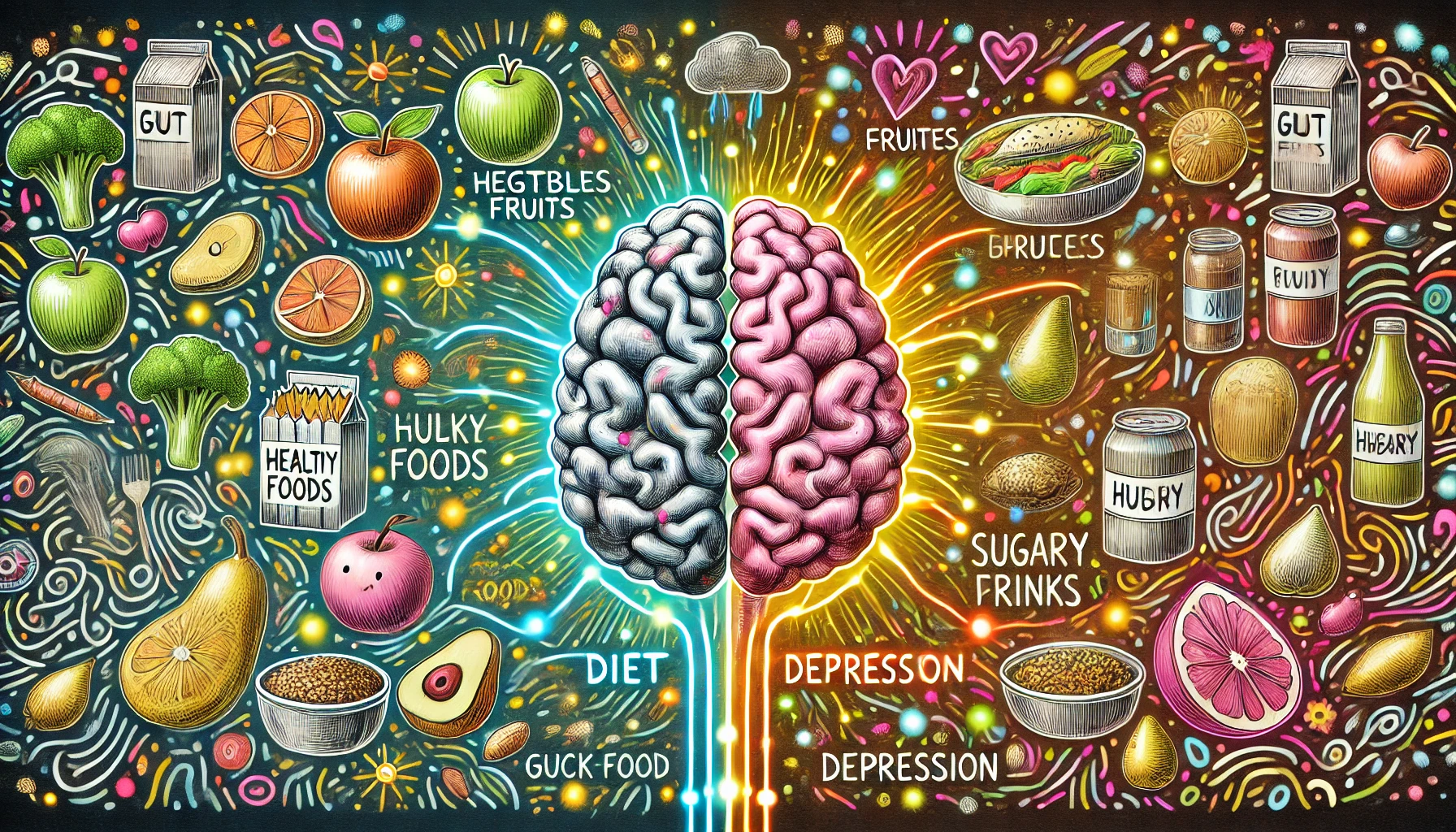
The relationship between diet and mental health has gained significant attention in recent years, particularly when it comes to depression. While many factors contribute to depressive disorders, the gut-brain connection has emerged as a key player in understanding how what we eat affects how we feel. The gut, often called the “second brain,” has its own nervous system, the enteric nervous system, which communicates directly with the brain. This communication happens via the gut-brain axis, a complex network involving neurotransmitters, hormones, and the immune system. More importantly, the gut hosts trillions of bacteria collectively known as the microbiome, which plays a vital role in both digestion and mental well-being. A balanced diet that nourishes the gut can positively impact mental health, while a poor diet can exacerbate symptoms of depression.
Dietary patterns influence the gut microbiome, which in turn affects the brain through the production of chemicals like serotonin, a neurotransmitter that regulates mood. Certain nutrients and food types can either support or undermine this process, making it crucial to examine the impact of diet on depression. Research has shown that gut bacteria produce up to 90% of the body’s serotonin, reinforcing the connection between gut health and mood regulation. This underscores the importance of consuming a diet that supports a healthy gut environment, which in turn can mitigate the risk of depression. In this blog, we will explore 10 key ways your diet impacts depression through the gut-brain connection.
1. Probiotics and Gut Health
- Probiotics are live bacteria found in fermented foods like yogurt, kefir, and sauerkraut. These “good” bacteria help balance the gut microbiome.
- Research suggests that an imbalance in gut bacteria, known as dysbiosis, can contribute to inflammation, which is linked to depression.
- Probiotics have been shown to improve mental health by reducing symptoms of depression and anxiety through their influence on gut flora.
- Including probiotic-rich foods in your diet can support gut health, potentially lowering the risk of developing depressive symptoms.
- Supplements can also help, but it’s always best to obtain probiotics from whole foods when possible.
2. Prebiotics and Mood
- Prebiotics are fibers that feed the beneficial bacteria in the gut, promoting a healthy microbiome.
- Foods rich in prebiotics include bananas, onions, garlic, and whole grains, which help maintain the balance of gut bacteria.
- Prebiotics have been linked to improved mood and reduced anxiety, likely due to their role in maintaining gut health.
- Supporting gut bacteria with prebiotics is essential for producing neurotransmitters that affect mood, like serotonin.
- Regular intake of prebiotics can enhance the benefits of probiotics, providing a synergistic effect on mental well-being.
3. Omega-3 Fatty Acids
- Omega-3s are essential fats found in fatty fish like salmon, mackerel, and sardines. They have anti-inflammatory properties crucial for brain health.
- Research indicates that low levels of omega-3s are associated with an increased risk of depression.
- Omega-3 fatty acids help maintain the structure of brain cells and support neurotransmitter function, including serotonin and dopamine.
- Regular consumption of omega-3-rich foods has been shown to reduce symptoms of depression and anxiety.
- Fish oil supplements can be an alternative for those who don’t consume enough omega-3s through diet alone.
4. Antioxidant-Rich Foods
- Oxidative stress in the brain is associated with depression. Antioxidants help combat this stress by neutralizing free radicals.
- Fruits and vegetables, especially berries, spinach, and kale, are rich in antioxidants like vitamin C and flavonoids.
- A diet high in antioxidants can protect the brain from inflammation and oxidative damage, which may reduce the risk of depression.
- Regular intake of antioxidant-rich foods helps maintain healthy brain function by protecting cells from damage.
- Incorporating a variety of colorful fruits and vegetables into your meals ensures a robust intake of antioxidants.
5. Complex Carbohydrates and Serotonin Production
- Carbohydrates are crucial for the production of serotonin, a key neurotransmitter for mood regulation.
- Complex carbs like whole grains, oats, and sweet potatoes provide a steady source of glucose, fueling the brain and maintaining mood stability.
- Simple carbs and sugar spikes, on the other hand, can lead to mood swings and energy crashes, which exacerbate symptoms of depression.
- Switching to complex carbohydrates ensures a steady release of energy, reducing the likelihood of mood dips.
- Including fiber-rich carbs supports gut health, which in turn fosters better serotonin production.
6. Vitamin D and Depression
- Vitamin D deficiency is commonly linked to mood disorders, including depression.
- The “sunshine vitamin” is found in fortified foods, fatty fish, and through direct sunlight exposure.
- Low levels of vitamin D can affect serotonin production, leading to depressive symptoms.
- Supplementing with vitamin D, especially during winter months, has been shown to improve mood and reduce depressive symptoms.
- Regular exposure to sunlight or a vitamin D supplement can support both mental health and immune function.
7. Magnesium and Mood Regulation
- Magnesium is a mineral involved in hundreds of biochemical reactions, including neurotransmitter function.
- Low magnesium levels are associated with an increased risk of depression and anxiety.
- Foods rich in magnesium, like leafy greens, nuts, seeds, and whole grains, support brain function and mood regulation.
- Magnesium can reduce stress by regulating the body’s response to it, making it an important nutrient for those at risk of depression.
- Regular magnesium intake through diet or supplements can improve overall mood and cognitive function.
8. Gut Inflammation and Processed Foods
- Processed foods are often high in sugar, unhealthy fats, and additives, which can trigger inflammation in the gut.
- Chronic gut inflammation has been linked to mood disorders, including depression.
- A diet high in processed foods can disrupt the balance of gut bacteria, contributing to mental health issues.
- Cutting back on processed foods and replacing them with whole, nutrient-dense options can significantly improve gut health and reduce depressive symptoms.
- Focus on reducing consumption of sugary snacks, fast food, and refined carbohydrates to improve mood stability.
9. Hydration and Mental Clarity
- Staying hydrated is crucial for brain function and mood regulation. Even mild dehydration can affect mental clarity and emotional stability.
- Water is necessary for every biological process, including the production of neurotransmitters that influence mood.
- Dehydration can lead to fatigue, headaches, and irritability, all of which can worsen symptoms of depression.
- Regular water intake, along with foods that have high water content like cucumbers and melons, supports mental health.
- Avoiding excessive caffeine and sugary drinks can help maintain hydration and improve mood.
10. Personalized Nutrition and Mental Health
- Individual responses to food can vary, and personalized nutrition approaches may be necessary to address specific mental health concerns.
- Food intolerances and sensitivities can contribute to inflammation and worsen depressive symptoms in some individuals.
- A personalized diet plan that takes into account food sensitivities, nutrient deficiencies, and lifestyle factors can support better mental health outcomes.
- Consulting with a nutritionist or healthcare provider can help tailor a diet that supports both physical and mental well-being.
- Tracking food intake and mood can help identify patterns and adjust dietary habits to improve mental health.
Conclusion
The connection between diet and depression through the gut-brain axis is clear. By understanding how certain foods and nutrients impact gut health and mood regulation, individuals can take steps toward improving their mental well-being. A balanced diet rich in probiotics, prebiotics, omega-3 fatty acids, antioxidants, and essential vitamins and minerals can foster a healthy gut environment and support optimal brain function. On the other hand, processed foods, poor hydration, and nutrient deficiencies can exacerbate depressive symptoms, making it essential to prioritize whole foods that nourish both the body and mind. Personalized nutrition approaches are also vital, as each individual’s gut-brain connection responds uniquely to dietary changes.
By making informed dietary choices, individuals can positively influence their mental health, reduce inflammation, and promote overall well-being. Focusing on gut health through nutrition can be a powerful tool in managing depression and supporting a healthier, happier life.