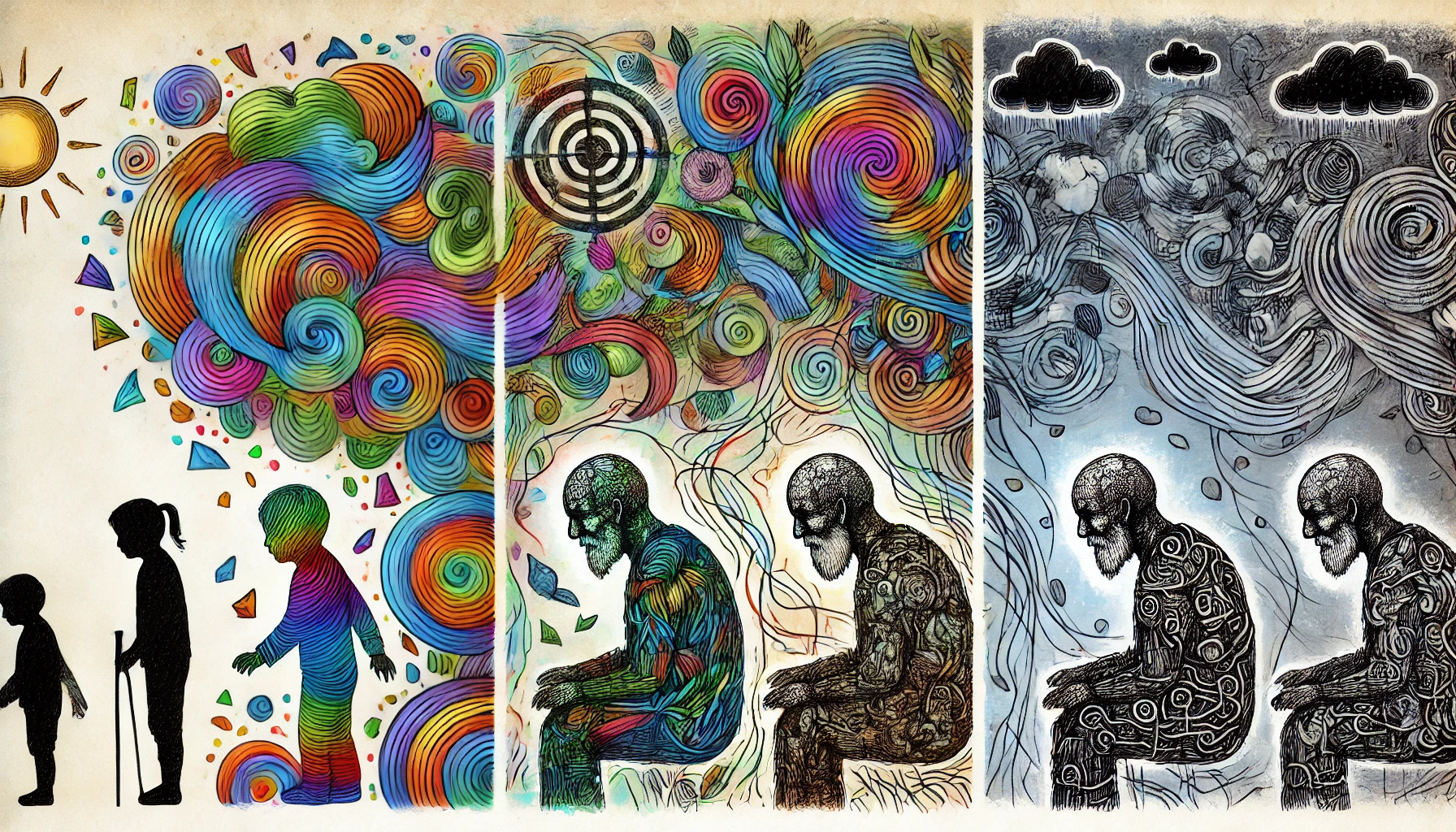
Depression is a pervasive mental health condition that affects individuals across all age groups, but it doesn’t manifest the same way in everyone. Factors such as age, developmental stage, and life experiences play a significant role in shaping how depression presents and impacts individuals. Understanding how depression differs across age groups is crucial for identifying the signs and providing appropriate support and treatment. This blog explores the nuances of depression in children, adolescents, adults, and older adults, highlighting the unique characteristics and challenges associated with each stage of life.
Depression in children might be confused with behavioral issues, while in adolescents, it can be mistaken for typical teenage angst. In adults, depression often intertwines with stress and responsibility, while in older adults, it might be overlooked as a part of aging. Recognizing these distinctions is essential for early intervention and effective management. By examining how depression manifests differently across age groups, we can better understand and support those affected at every stage of life.
Depression in Children
- Behavioral Changes
- In children, depression often manifests as irritability, anger, or disruptive behavior rather than sadness. These behavioral changes can be mistaken for disciplinary issues or developmental phases.
- Children may become more clingy, fearful, or refuse to go to school, which can be interpreted as separation anxiety or behavioral problems.
- They might display a lack of interest in play or activities they once enjoyed, which is often a subtle sign of an underlying mood disorder.
- Sleep disturbances, such as nightmares or difficulty falling asleep, are common in depressed children, affecting their overall well-being.
- Early identification is crucial, as untreated depression in childhood can lead to long-term emotional and developmental issues.
- Physical Complaints
- Children with depression often report physical symptoms like stomachaches, headaches, or other unexplained aches and pains.
- These physical complaints can be a child’s way of expressing emotional distress when they lack the vocabulary to articulate their feelings.
- Frequent visits to the school nurse or a decline in school performance may indicate that a child is struggling with emotional issues.
- Children may also exhibit changes in appetite, either eating too much or too little, which can affect their physical growth and development.
- Parents and caregivers should take these physical symptoms seriously, as they can be early indicators of depression.
Depression in Adolescents
- Mood Swings and Irritability
- Adolescents with depression may exhibit significant mood swings, ranging from irritability and anger to withdrawal and apathy. These shifts are often more pronounced than typical teenage moodiness.
- Irritability, rather than sadness, is frequently a dominant symptom in depressed teens, leading to conflicts with peers, family members, and authority figures.
- Adolescents may become hypersensitive to criticism and express feelings of worthlessness or inadequacy, impacting their self-esteem.
- Emotional outbursts or a constant sense of frustration can mask underlying depression, making it difficult for parents and teachers to identify.
- Open communication and active listening are essential to support teens, as they may struggle to express their emotions directly.
- Risky Behaviors and Substance Use
- Depression in adolescents can lead to an increase in risky behaviors, such as experimenting with drugs or alcohol, reckless driving, or engaging in unsafe sexual practices.
- These behaviors can be a form of self-medication or a way to cope with emotional pain and the overwhelming feelings associated with depression.
- Adolescents may also engage in self-harm or express suicidal thoughts, highlighting the need for immediate intervention and support.
- Substance abuse can complicate the diagnosis and treatment of depression, as it may exacerbate mood symptoms and lead to a cycle of dependency.
- Early intervention is key to preventing these behaviors from escalating and addressing the underlying depressive symptoms.
Depression in Adults
- Functional Impairment
- In adults, depression often presents as a decline in functioning, affecting work performance, social interactions, and daily responsibilities.
- Adults may experience difficulty concentrating, making decisions, or remembering details, which can impact their professional and personal lives.
- Feelings of exhaustion and a lack of motivation can make it challenging to complete daily tasks, leading to neglect of self-care, household duties, or job responsibilities.
- This impairment can result in a cycle of decreased productivity and increased stress, further exacerbating depressive symptoms.
- Seeking professional help, such as therapy or medication, is important for managing these impairments and improving quality of life.
- Chronic Stress and Life Events
- Adult depression is often triggered or worsened by life events such as job loss, financial strain, relationship problems, or the death of a loved one.
- The responsibilities of adulthood, including career pressures and family obligations, can contribute to the onset or persistence of depressive symptoms.
- Chronic stress can lead to burnout, a state of emotional, mental, and physical exhaustion that overlaps with symptoms of depression.
- Unlike adolescents, adults may not always display overt signs of distress, as they might internalize their struggles and try to maintain a façade of coping.
- Recognizing the impact of life stressors and providing support can help mitigate the risk of depression in adults.
Depression in Older Adults
- Physical Health and Comorbidity
- Depression in older adults often coexists with physical health problems such as chronic pain, heart disease, or neurological conditions like Parkinson’s or Alzheimer’s disease.
- Physical symptoms like fatigue, sleep disturbances, and appetite changes are common and can be mistaken for normal aging rather than signs of depression.
- Older adults may be less likely to report feelings of sadness and instead present with somatic complaints, such as unexplained aches, gastrointestinal issues, or general malaise.
- The presence of comorbid medical conditions can complicate the diagnosis and treatment of depression, requiring a comprehensive approach to care.
- Proper screening and assessment are crucial, as treating depression in older adults can improve overall health outcomes and quality of life.
- Social Isolation and Loss
- Social isolation is a significant risk factor for depression in older adults, especially for those who live alone or have limited social support.
- The loss of loved ones, retirement, or a decline in physical abilities can lead to feelings of loneliness, grief, and a loss of purpose.
- Older adults may experience a sense of hopelessness or helplessness, particularly if they feel they are a burden to others or have lost their independence.
- Encouraging social engagement, whether through community activities, support groups, or family interactions, is essential for mental well-being in this age group.
- Interventions such as therapy, social support, and lifestyle changes can help alleviate the impact of social isolation and loss on depression.
Suicide Risk Across Age Groups
- Suicidal Ideation in Adolescents
- Adolescents are particularly vulnerable to suicidal thoughts and behaviors due to the intensity of their emotions and the developmental challenges they face.
- The presence of depression, combined with factors such as bullying, academic pressure, or family conflict, can increase the risk of suicidal ideation in teens.
- Warning signs include talking about death, giving away possessions, or expressing feelings of hopelessness or being trapped.
- Immediate intervention and support are critical for adolescents exhibiting signs of suicidal ideation, including seeking professional help and ensuring a supportive environment.
- Prevention strategies involve open communication, mental health education, and access to counseling services.
- Suicide Risk in Older Adults
- Older adults, particularly men over the age of 65, have a higher risk of suicide, often related to factors such as chronic illness, loss of independence, or social isolation.
- Depression in older adults may be overlooked or dismissed as a normal part of aging, leading to a lack of appropriate support and intervention.
- Suicidal ideation in this age group may be expressed subtly, through statements like “I feel like a burden” or “I’m tired of living.”
- Healthcare providers and caregivers must be vigilant in assessing the mental health of older adults and addressing any signs of depression or suicidal thoughts.
- Providing a strong support system, regular mental health check-ups, and access to mental health resources can help reduce the risk of suicide in older adults.
Conclusion
Depression manifests differently across age groups, influenced by developmental stages, life circumstances, and social environments. In children, it often presents as behavioral changes and physical complaints, while in adolescents, it may involve mood swings, irritability, and risky behaviors. Adults may experience functional impairment and chronic stress, and in older adults, depression can be complicated by physical health issues and social isolation. Understanding these differences is crucial for identifying the signs of depression early and providing age-appropriate support and treatment.
Recognizing the unique ways depression can manifest in each age group allows for more targeted interventions and a better chance of successful outcomes. Early detection and treatment are vital for preventing the progression of depression and improving the quality of life for individuals at every stage. By fostering awareness and understanding, we can create a more supportive environment for those affected by depression, regardless of their age.