Heart attacks, or myocardial infarctions, occur when blood flow to a part of the heart is blocked, causing damage to the heart muscle. They are a major medical emergency and a leading cause of death worldwide. However, contrary to popular belief, not all heart attacks present with the same symptoms. The classic image of a person clutching their chest in pain is just one of many possible presentations. In reality, symptoms can vary significantly depending on factors such as age, gender, underlying health conditions, and the type of heart attack.
Understanding the range of heart attack symptoms is crucial for timely diagnosis and treatment. This blog explores the different types of heart attack symptoms, highlighting how they can manifest in various ways. We aim to provide a comprehensive overview to help individuals recognize potential signs and seek prompt medical attention.
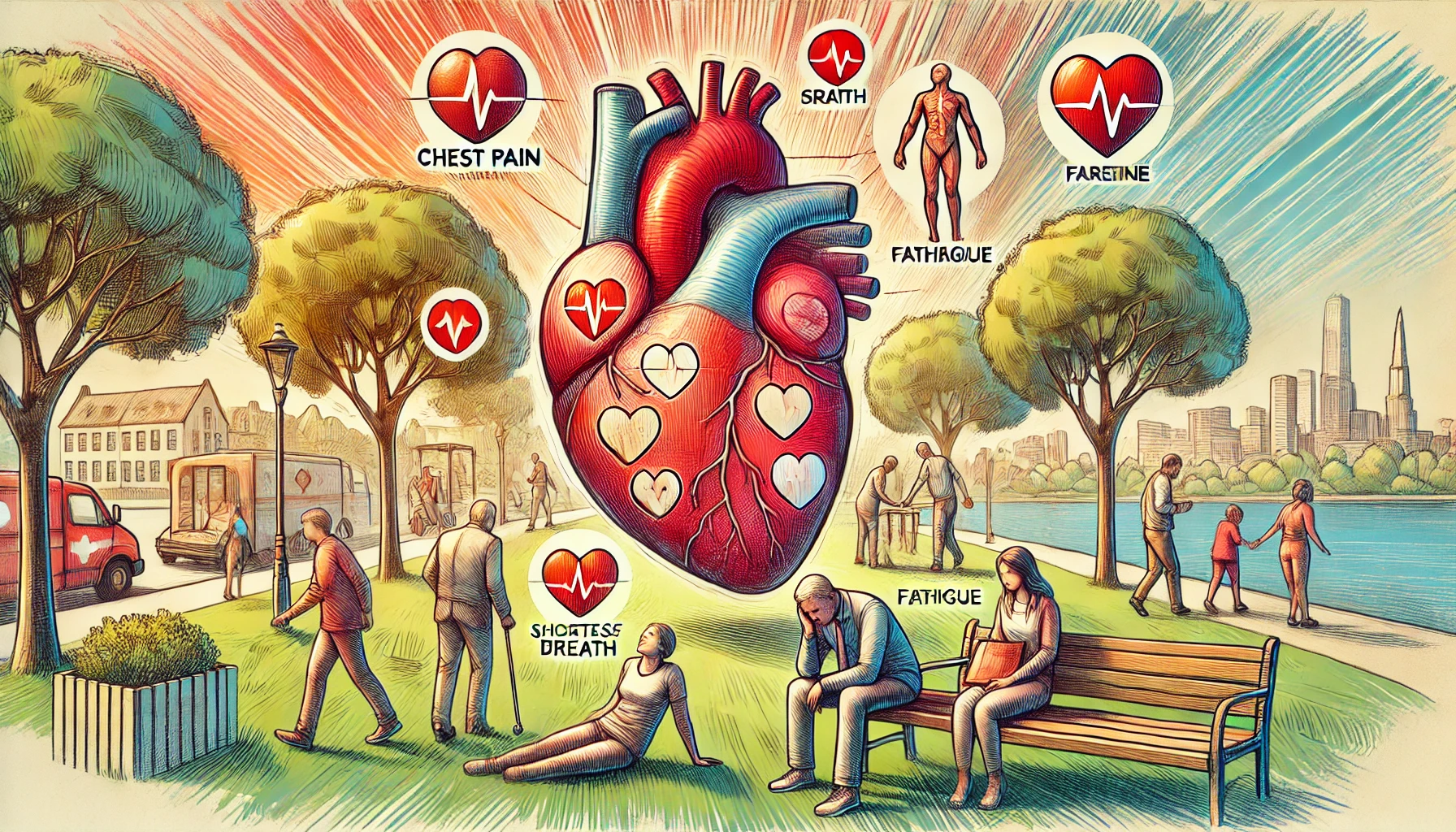
1. Classic Symptoms of a Heart Attack
- Chest Pain or Discomfort: Often described as a squeezing, pressure, fullness, or pain in the center of the chest. It can last for more than a few minutes or come and go.
- Radiating Pain: Pain may radiate to the shoulders, arms (especially the left arm), back, neck, jaw, or stomach.
- Shortness of Breath: Difficulty breathing, which may occur with or without chest discomfort.
- Nausea and Vomiting: Feeling nauseous or vomiting can be a symptom of a heart attack, especially in women.
- Cold Sweats: Sudden sweating without obvious cause can be a sign of a heart attack.
2. Atypical Symptoms of a Heart Attack
- Indigestion or Heartburn: Some people may mistake a heart attack for indigestion, heartburn, or a stomach ulcer.
- Fatigue: Unusual tiredness or fatigue, especially if it comes on suddenly or is unexplained.
- Dizziness or Lightheadedness: Feeling dizzy or lightheaded can occur, sometimes accompanied by fainting.
- Anxiety or Panic: A sudden feeling of intense anxiety or a sense of impending doom.
- Palpitations: Irregular heartbeats or a feeling that the heart is pounding or fluttering.
3. Silent Heart Attacks
- Definition: A silent heart attack occurs without noticeable symptoms. It is more common in people with diabetes or in older adults.
- Detection: Often discovered during routine check-ups, ECGs, or when investigating other health issues.
- Risk Factors: High blood pressure, diabetes, and a history of heart disease increase the risk of silent heart attacks.
- Significance: Despite the lack of symptoms, silent heart attacks can cause damage to the heart muscle and increase the risk of future cardiovascular events.
- Prevention and Monitoring: Regular medical check-ups and monitoring of heart health can help detect silent heart attacks.
4. Differences in Symptoms Between Men and Women
- Men: More likely to experience classic symptoms like chest pain, pressure, or discomfort that radiates to the arm.
- Women: More likely to experience atypical symptoms such as shortness of breath, nausea, vomiting, back or jaw pain, and extreme fatigue.
- Underrecognition: Women’s symptoms are sometimes underrecognized, leading to delayed treatment and worse outcomes.
- Awareness and Education: Increasing awareness of how heart attack symptoms can differ between genders is crucial for timely diagnosis and treatment.
- Clinical Implications: Healthcare providers should consider gender-specific symptoms when diagnosing heart attacks.
5. Heart Attack Symptoms in Older Adults
- Subtle Symptoms: Older adults may experience less intense or atypical symptoms, such as shortness of breath, fatigue, or weakness.
- Confusion or Cognitive Impairment: Acute confusion or cognitive impairment can sometimes be the primary symptom in older adults.
- Coexisting Conditions: Other medical conditions, such as arthritis or diabetes, may mask or complicate heart attack symptoms.
- Communication Challenges: Older adults may underreport symptoms or attribute them to aging or other health issues.
- Importance of Vigilance: Family members and caregivers should be vigilant for subtle signs of a heart attack in older adults.
6. Heart Attack Symptoms in Diabetics
- Neuropathy: Diabetes-related nerve damage can lead to reduced pain perception, resulting in milder or atypical symptoms.
- Silent Heart Attacks: Diabetics have a higher risk of silent heart attacks due to neuropathy.
- Common Symptoms: Symptoms can include shortness of breath, fatigue, dizziness, and sweating.
- Increased Risk: Diabetics have a higher risk of heart disease and complications, making early detection critical.
- Regular Monitoring: Routine check-ups and cardiovascular screenings are essential for diabetics to detect heart issues early.
7. The Role of Pre-Existing Conditions
- Angina: People with a history of angina may experience similar chest pain during a heart attack, making it challenging to distinguish between the two.
- Heart Failure: Those with heart failure may experience worsening symptoms, such as increased shortness of breath or swelling.
- Previous Heart Attacks: A history of heart attacks increases the risk of recurrence, and symptoms may vary with each episode.
- Chronic Obstructive Pulmonary Disease (COPD): COPD can exacerbate symptoms like shortness of breath, making it harder to identify a heart attack.
- Importance of Medical History: A comprehensive medical history helps healthcare providers assess and diagnose heart attack symptoms accurately.
8. Psychological Factors and Heart Attack Symptoms
- Anxiety Disorders: Individuals with anxiety disorders may experience symptoms that mimic heart attacks, such as chest pain or palpitations.
- Stress and Panic Attacks: Acute stress or panic attacks can cause chest pain and other symptoms similar to a heart attack.
- Misinterpretation: Psychological factors can lead to misinterpretation of symptoms, causing individuals to delay seeking medical attention.
- Mind-Body Connection: The psychological state can influence the perception of pain and other physical symptoms.
- Importance of Comprehensive Assessment: Healthcare providers should consider psychological factors when assessing heart attack symptoms.
9. When to Seek Medical Attention
- Immediate Action: Seek immediate medical attention if experiencing chest pain, shortness of breath, or any other concerning symptoms.
- Don’t Ignore Symptoms: Even if symptoms seem mild or atypical, they should not be ignored, as they could indicate a heart attack.
- Emergency Services: Call emergency services rather than driving to the hospital, as paramedics can begin treatment en route.
- Time Is Muscle: Prompt treatment is critical in minimizing heart damage and improving outcomes.
- Communication: Clearly describe symptoms to healthcare providers to aid in accurate diagnosis and treatment.
10. Prevention and Awareness
- Know Your Risk: Understand personal risk factors for heart disease, including family history, lifestyle, and pre-existing conditions.
- Healthy Lifestyle: Maintain a heart-healthy lifestyle with regular exercise, a balanced diet, and no smoking.
- Regular Check-Ups: Regular medical check-ups can help detect and manage risk factors like hypertension, high cholesterol, and diabetes.
- Stress Management: Manage stress through healthy practices like mindfulness, relaxation techniques, and physical activity.
- Education and Awareness: Educate yourself and others about the signs and symptoms of heart attacks to promote early detection and treatment.
Conclusion
Not all heart attacks have the same symptoms, and they can vary widely depending on several factors, including age, gender, underlying health conditions, and the type of heart attack. Understanding the range of possible symptoms is crucial for recognizing a heart attack and seeking timely medical intervention. While classic symptoms like chest pain are common, atypical presentations can also indicate a heart attack, particularly in women, older adults, and people with diabetes.
Awareness and education are vital for early detection and treatment, which can significantly improve outcomes and reduce the risk of complications. Maintaining a heart-healthy lifestyle, being aware of personal risk factors, and knowing when to seek medical attention are essential steps in protecting your heart health.