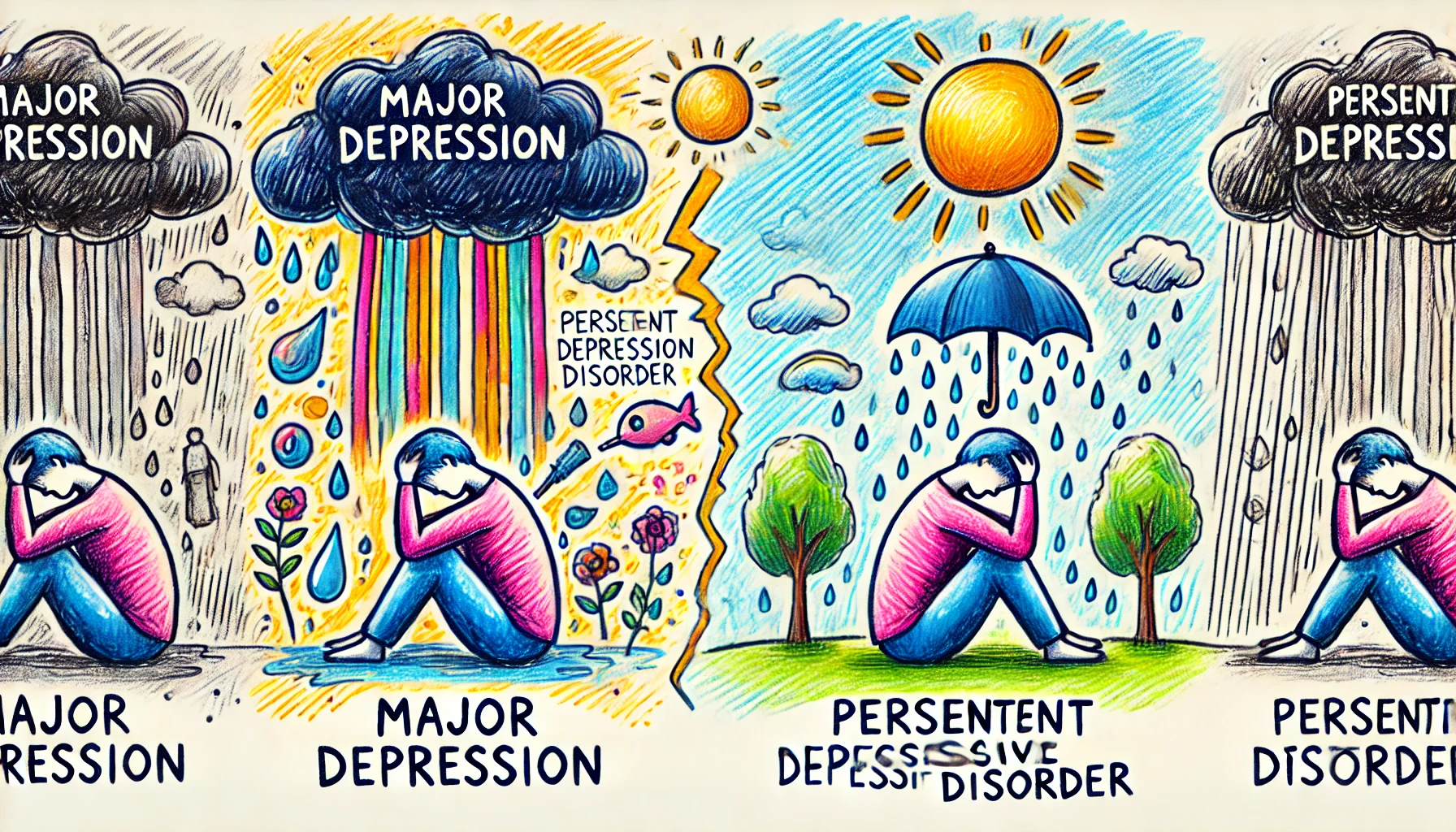
Depression is a complex mental health condition that affects millions of people worldwide. Within the spectrum of depressive disorders, two common types often discussed are Major Depressive Disorder (MDD) and Persistent Depressive Disorder (PDD). While they share some similarities, such as symptoms of sadness and a loss of interest in daily activities, they differ in their duration, intensity, and impact on a person’s life. Understanding these distinctions is crucial for effective diagnosis and treatment.
Major Depressive Disorder is often characterized by intense, severe episodes of depression that can significantly impair an individual’s ability to function in daily life. These episodes can be debilitating, leading to profound emotional and physical symptoms. On the other hand, Persistent Depressive Disorder, previously known as dysthymia, involves a chronic, long-lasting form of depression. PDD symptoms are usually less severe but are more enduring, often lasting for years. This blog will explore the key differences between these two disorders to enhance awareness and understanding.
1. Duration of Symptoms
- Major Depressive Disorder: The symptoms last for at least two weeks but can extend for several months if untreated. MDD episodes are often episodic, with periods of normal mood in between.
- Persistent Depressive Disorder: Symptoms must be present for at least two years in adults or one year in children and adolescents. PDD is characterized by a chronic course with symptoms that persist most of the day, more days than not.
- Relapse and Remission: MDD can have multiple episodes throughout a person’s life, with periods of remission in between. In contrast, PDD is more continuous and does not have clearly defined episodes.
- Severity Over Time: While MDD symptoms can come and go, PDD symptoms tend to remain relatively consistent over time, with fluctuations in severity but without full remission.
- Impact on Daily Life: Due to its chronic nature, PDD can often lead to long-term functional impairment, whereas MDD can cause intense, acute disruptions in daily functioning during episodes.
2. Severity of Symptoms
- Major Depressive Disorder: MDD is marked by severe symptoms, including deep sadness, hopelessness, significant weight changes, sleep disturbances, and thoughts of death or suicide. These symptoms can be intense and overwhelming.
- Persistent Depressive Disorder: PDD symptoms are typically less severe than those of MDD but are more persistent. Common symptoms include low self-esteem, feelings of inadequacy, and a lack of energy or enthusiasm.
- Functionality: While PDD allows for some level of daily functioning, albeit with a constant low mood, MDD often makes it difficult to perform even basic tasks, affecting work, relationships, and daily responsibilities.
- Emotional Impact: MDD can cause significant emotional pain and distress, often leading to a sense of worthlessness or guilt. PDD, while more chronic, can create an ongoing sense of pessimism or lack of joy in life.
- Intensity Variations: MDD’s intensity can vary significantly from person to person, with some experiencing psychotic symptoms such as delusions or hallucinations, which is less common in PDD.
3. Onset and Development
- Major Depressive Disorder: MDD can develop at any age, but the average onset is in the mid-20s. It can be triggered by life events, trauma, or biological factors. The onset can be sudden, with symptoms appearing rapidly.
- Persistent Depressive Disorder: PDD often begins earlier in life, with many individuals reporting symptoms in childhood or adolescence. The onset is usually more gradual and less severe initially.
- Early Life Factors: Early life stressors, such as childhood trauma or family history of depression, can increase the risk of developing either disorder, but they are more commonly associated with PDD.
- Gender Differences: Women are more likely to be diagnosed with both MDD and PDD, possibly due to hormonal, genetic, or psychosocial factors. This difference in gender prevalence is more pronounced in MDD.
- Progression: MDD can occur as a single episode or be recurrent, with periods of normal mood in between. PDD, on the other hand, is characterized by its chronic nature and slow progression.
4. Impact on Daily Functioning
- Major Depressive Disorder: MDD can severely impact daily functioning, often leading to a complete inability to work, socialize, or care for oneself. It can cause significant disruptions in daily life and relationships.
- Persistent Depressive Disorder: PDD allows for a greater level of functioning, although individuals often feel like they are merely “going through the motions.” The quality of life is usually diminished, but not to the same extent as in MDD.
- Social Impact: Both disorders can lead to social withdrawal, but MDD’s impact is usually more abrupt and noticeable. PDD might lead to a gradual distancing from social activities over time.
- Work and Productivity: MDD can result in significant absenteeism or inability to maintain employment. PDD may lead to reduced productivity and a lack of motivation at work.
- Coping Strategies: Individuals with PDD often develop coping mechanisms to deal with their symptoms, while those with MDD may struggle to cope during intense depressive episodes.
5. Diagnosis Criteria
- Major Depressive Disorder: According to the DSM-5, a diagnosis of MDD requires at least five symptoms (such as depressed mood, loss of interest, weight changes, sleep disturbances, fatigue, feelings of worthlessness, and suicidal ideation) to be present for a minimum of two weeks.
- Persistent Depressive Disorder: For PDD, the DSM-5 criteria require a depressed mood for most of the day, more days than not, for at least two years, along with at least two additional symptoms like poor appetite, low energy, low self-esteem, or hopelessness.
- Overlap in Diagnosis: It is possible for individuals to be diagnosed with both disorders, known as “double depression,” where a person with PDD experiences an MDD episode.
- Clinical Assessment: Diagnosis typically involves a thorough clinical assessment, including a psychiatric evaluation and discussion of the patient’s history, to differentiate between MDD and PDD.
- Rule Out Other Conditions: Diagnosing MDD and PDD involves ruling out other potential causes for symptoms, such as substance abuse, medical conditions, or other mental health disorders.
6. Treatment Approaches
- Major Depressive Disorder: Treatment for MDD often involves a combination of antidepressant medications (such as SSRIs, SNRIs, or tricyclics) and psychotherapy, including cognitive-behavioral therapy (CBT) or interpersonal therapy.
- Persistent Depressive Disorder: PDD treatment also includes antidepressants and psychotherapy. However, treatment is often longer-term due to the chronic nature of the disorder.
- Psychotherapy Focus: In PDD, therapy may focus on developing coping strategies and improving self-esteem, while in MDD, it may target symptom relief and crisis management.
- Lifestyle Modifications: Both disorders benefit from lifestyle changes such as regular exercise, healthy eating, sleep hygiene, and stress management techniques.
- Treatment Response: Individuals with MDD may respond to treatment more quickly, while those with PDD may require a longer and more sustained approach to see significant improvements.
7. Risk of Suicide
- Major Depressive Disorder: MDD is associated with a higher risk of suicide, particularly during severe episodes. This risk increases if there are co-occurring conditions like substance abuse or anxiety.
- Persistent Depressive Disorder: While the risk of suicide is lower in PDD compared to MDD, it still exists, especially in individuals with a long history of depressive symptoms or those who also experience episodes of MDD.
- Warning Signs: MDD often presents with more overt signs of suicidality, such as expressing a desire to die or making suicide attempts. In PDD, the signs may be more subtle and involve a chronic sense of hopelessness.
- Preventative Measures: Both conditions require careful monitoring and intervention to prevent suicide, including regular mental health evaluations and access to crisis support services.
- Family and Social Support: Strong social and family support networks can be crucial in reducing the risk of suicide in individuals with either MDD or PDD.
8. Prognosis and Long-Term Outlook
- Major Depressive Disorder: With proper treatment, many individuals with MDD can achieve full remission. However, there is a high risk of recurrence, especially if treatment is discontinued prematurely.
- Persistent Depressive Disorder: PDD is more challenging to treat due to its chronic nature. Individuals may experience symptoms for many years, even with treatment, but therapy can help improve the quality of life and functioning.
- Chronic Course: PDD’s chronic course means that individuals may need ongoing treatment and support, whereas MDD may be managed with shorter-term interventions between episodes.
- Factors Influencing Prognosis: The prognosis for both disorders can be influenced by factors such as the severity and duration of symptoms, treatment adherence, and the presence of supportive relationships.
- Importance of Early Intervention: Early diagnosis and intervention can improve the long-term outlook for both MDD and PDD, reducing the risk of complications and enhancing the quality of life.
9. Co-occurring Disorders
- Major Depressive Disorder: MDD often co-occurs with other mental health disorders, such as anxiety disorders, substance use disorders, and post-traumatic stress disorder (PTSD).
- Persistent Depressive Disorder: PDD can co-occur with anxiety disorders, personality disorders, and substance abuse. These co-occurring conditions can complicate the diagnosis and treatment process.
- Impact on Treatment: The presence of co-occurring disorders can affect treatment plans, requiring a more integrated approach that addresses multiple conditions simultaneously.
- Differentiating Symptoms: Clinicians must carefully differentiate symptoms of MDD and PDD from those of other co-occurring conditions to ensure an accurate diagnosis and effective treatment.
- Holistic Approach: A holistic treatment approach that considers the individual’s overall mental health and well-being is crucial for managing co-occurring disorders alongside MDD or PDD.
10. Quality of Life and Daily Functioning
- Major Depressive Disorder: MDD can severely impact the quality of life, leading to a loss of interest in activities, social isolation, and a decline in physical health due to poor self-care.
- Persistent Depressive Disorder: PDD’s impact on quality of life is more insidious, as individuals often adapt to their chronic symptoms, leading to a persistent state of dissatisfaction and underachievement.
- Relationship Strain: Both disorders can strain relationships, but MDD’s impact is often more acute and immediate, while PDD may lead to long-term issues due to ongoing emotional distance and lack of engagement.
- Physical Health: Both MDD and PDD are associated with a higher risk of physical health problems, such as cardiovascular disease and weakened immune function, due to the stress and lifestyle factors associated with chronic depression.
- Strategies for Improvement: Improving quality of life involves a comprehensive treatment plan, including medication, therapy, lifestyle changes, and support networks to help individuals regain a sense of purpose and fulfillment.
Conclusion
Understanding the differences between Major Depressive Disorder and Persistent Depressive Disorder is crucial for appropriate diagnosis, treatment, and management. While both are serious conditions that significantly impact a person’s life, they differ in terms of duration, severity, onset, and treatment approach. MDD is often characterized by intense, episodic depressive episodes that can be debilitating, while PDD involves a chronic, long-lasting depressive state that may be less severe but is more persistent. Recognizing these differences can help individuals and healthcare professionals develop more effective, individualized treatment plans.
Effective management of both disorders involves a combination of medication, psychotherapy, lifestyle modifications, and support from family and social networks. Early intervention and ongoing support are key to improving the long-term outlook for individuals with MDD and PDD, helping them achieve a better quality of life and reducing the risk of complications such as suicide and co-occurring disorders. By increasing awareness and understanding of these conditions, we can work towards more compassionate and effective care for those affected by depression.