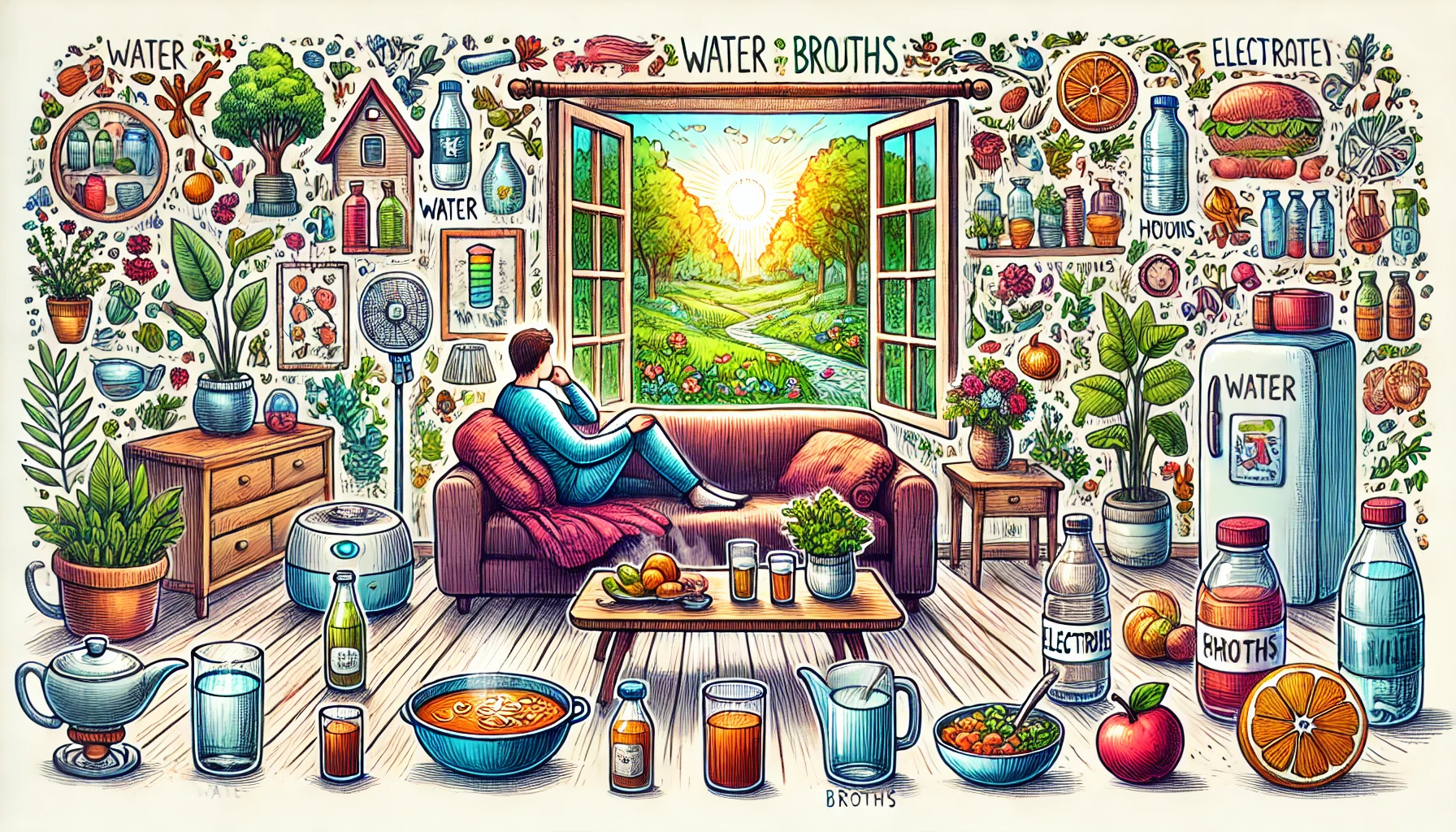
Staying hydrated is crucial for maintaining health, and it becomes even more important during illness. Illnesses often lead to increased fluid loss due to fever, vomiting, diarrhea, or decreased fluid intake because of discomfort and lack of appetite. Proper hydration supports the immune system, helps regulate body temperature, and facilitates the elimination of toxins. This blog will guide you through the best practices and tips for staying hydrated during illness, ensuring your body has the fluids it needs to recover efficiently.
When you’re feeling under the weather, your body’s demand for fluids increases significantly. Fever, one of the body’s natural responses to infection, can cause substantial fluid loss through sweating. Gastrointestinal illnesses, such as stomach flu, can lead to dehydration through vomiting and diarrhea. Even respiratory infections can increase fluid needs due to mucus production and the potential for fever. Therefore, understanding how to stay adequately hydrated during illness is essential for a quicker and smoother recovery.
1. Recognize the Signs of Dehydration
- Dry Mouth and Thirst: One of the earliest and most obvious signs of dehydration is a dry mouth and an increased feeling of thirst.
- Dark Urine: Urine color is a good indicator; dark yellow or amber urine often signifies dehydration.
- Fatigue and Weakness: Dehydration can lead to feelings of fatigue and general weakness, making it harder to recover from illness.
- Dizziness or Lightheadedness: Feeling dizzy or lightheaded can indicate that your body is not getting enough fluids.
- Reduced Urine Output: Dehydrated individuals tend to urinate less frequently, and the urine is usually more concentrated.
2. Drink Small Amounts Frequently
- Sips Instead of Gulps: Taking small sips of fluid regularly can be more effective and tolerable than drinking large amounts at once.
- Set a Schedule: Create a hydration schedule to remind yourself to drink fluids regularly, even if you don’t feel thirsty.
- Use a Straw: Sometimes using a straw can make it easier to take in fluids, especially if you’re feeling nauseous.
- Cool or Warm Liquids: Depending on your symptoms, you might find that cool or warm liquids are more soothing and easier to drink.
- Variety of Fluids: Mix up your fluid intake with a variety of drinks to prevent monotony and encourage consistent hydration.
3. Choose Hydrating Foods
- Broths and Soups: Clear broths and soups are excellent choices as they provide both hydration and essential nutrients.
- Fruits and Vegetables: Foods with high water content, such as watermelon, cucumber, and oranges, contribute to overall hydration.
- Gelatin and Popsicles: These can be soothing on the throat and provide a source of fluids.
- Electrolyte-Rich Foods: Foods like bananas and avocados can help replenish electrolytes lost through vomiting or diarrhea.
- Yogurt: This can be gentle on the stomach and provide hydration as well as beneficial probiotics.
4. Incorporate Electrolyte Solutions
- Oral Rehydration Solutions (ORS): Specially formulated ORS can be highly effective in preventing and treating dehydration.
- Sports Drinks: These can be useful for short-term rehydration, particularly if they contain low sugar and added electrolytes.
- Homemade Solutions: A simple homemade electrolyte solution can be made with water, salt, and sugar.
- Pediatric Electrolyte Drinks: These are designed to be gentle on the stomach and effective for hydration.
- Coconut Water: A natural alternative that provides electrolytes and hydration without added sugars.
5. Avoid Dehydrating Beverages
- Caffeinated Drinks: Coffee, tea, and sodas can have a diuretic effect, potentially exacerbating dehydration.
- Alcohol: Alcohol can significantly increase fluid loss and should be avoided during illness.
- Sugary Drinks: High sugar content can lead to further dehydration and should be consumed in moderation or avoided.
- Highly Acidic Drinks: Citrus juices and other acidic drinks can irritate the stomach and should be limited.
- Energy Drinks: Often high in caffeine and sugar, these are not recommended for hydration during illness.
6. Use Hydration Aids
- Hydration Tablets: Dissolvable tablets that can be added to water, providing a boost of electrolytes and flavor.
- Hydration Packs: Pre-made packs that mix with water to create an electrolyte-rich drink.
- Nasal Sprays: Saline nasal sprays can help maintain mucosal hydration, particularly with respiratory illnesses.
- Humidifiers: Using a humidifier can keep the air moist and help maintain overall hydration, especially useful during respiratory infections.
- Hydration Apps: Apps can track your fluid intake and remind you to drink regularly.
7. Rest and Recovery
- Stay Cool: Keep your environment cool to reduce fluid loss through sweating if you have a fever.
- Comfortable Environment: Ensure you have a comfortable space to rest, promoting relaxation and reducing stress on the body.
- Elevate Feet: Elevating your feet can improve circulation and help with overall recovery.
- Avoid Overexertion: Rest as much as possible to allow your body to focus on fighting the illness and maintaining hydration.
- Sleep: Quality sleep can significantly aid in recovery and hydration management.
8. Monitor Your Fluid Intake
- Track Consumption: Use a journal or app to keep track of how much fluid you’re consuming each day.
- Set Goals: Set daily hydration goals based on your weight and level of illness to ensure adequate intake.
- Measure Fluid Loss: Pay attention to fluid loss through sweating, urination, vomiting, or diarrhea and adjust intake accordingly.
- Check Weight: Sudden weight loss can indicate dehydration; regular weight checks can help monitor this.
- Seek Help if Needed: If you’re unable to keep fluids down, seek medical advice to prevent severe dehydration.
9. Seek Medical Advice
- Professional Guidance: Consult with healthcare providers to get personalized advice based on your illness and hydration needs.
- Medications: Some medications can affect hydration, and a doctor can advise on any necessary adjustments.
- IV Fluids: In severe cases of dehydration, intravenous fluids might be necessary for proper rehydration.
- Follow-Up: Regular follow-ups can help ensure that you are on the right track with your hydration and recovery.
- Tailored Plan: A healthcare provider can create a tailored hydration plan that considers your specific symptoms and medical history.
10. Educate Yourself and Loved Ones
- Understanding Needs: Learn about your body’s hydration needs, especially during illness, to better manage fluid intake.
- Teach Others: Share knowledge with family and friends to help them stay hydrated during their own illnesses.
- Emergency Preparedness: Keep oral rehydration solutions and electrolyte drinks at home for quick access during illnesses.
- Hydration Techniques: Learn and practice different hydration techniques that work best for you.
- Stay Informed: Keep up with the latest information on hydration and health to stay well-prepared for any future illnesses.
Maintaining proper hydration during illness is essential for a swift and effective recovery. Recognizing the signs of dehydration, drinking small amounts frequently, incorporating hydrating foods, and choosing electrolyte solutions are key steps. Avoiding dehydrating beverages, using hydration aids, and seeking medical advice when necessary can further ensure that you stay well-hydrated. Educating yourself and others about hydration needs can also play a significant role in managing health during illnesses. By following these strategies, you can support your body’s recovery process and maintain optimal health during times of sickness.